Many unnecessary hospitalizations occur due to poor communication. These hospitalizations can often be avoided by calling the medical provider in a timely fashion with a complete report.
When you call a provider to give them an update on a patient’s condition, they will usually want a brief, to the point explanation of what is going on. The doctor will need the information that will allow them to treat the patient properly.
Once they have the information they need, they will usually give orders or approve things that need to be done. Sometimes it may be a simple update that doesn’t require any further questions or data points.
What kind of system should you use to prepare to give a report?
Reporting should follow some system that allows you to have the information needed for the medical provider to make a decision. Whatever method you use to gather your information, you will need to make sure it prepares you to make the call.
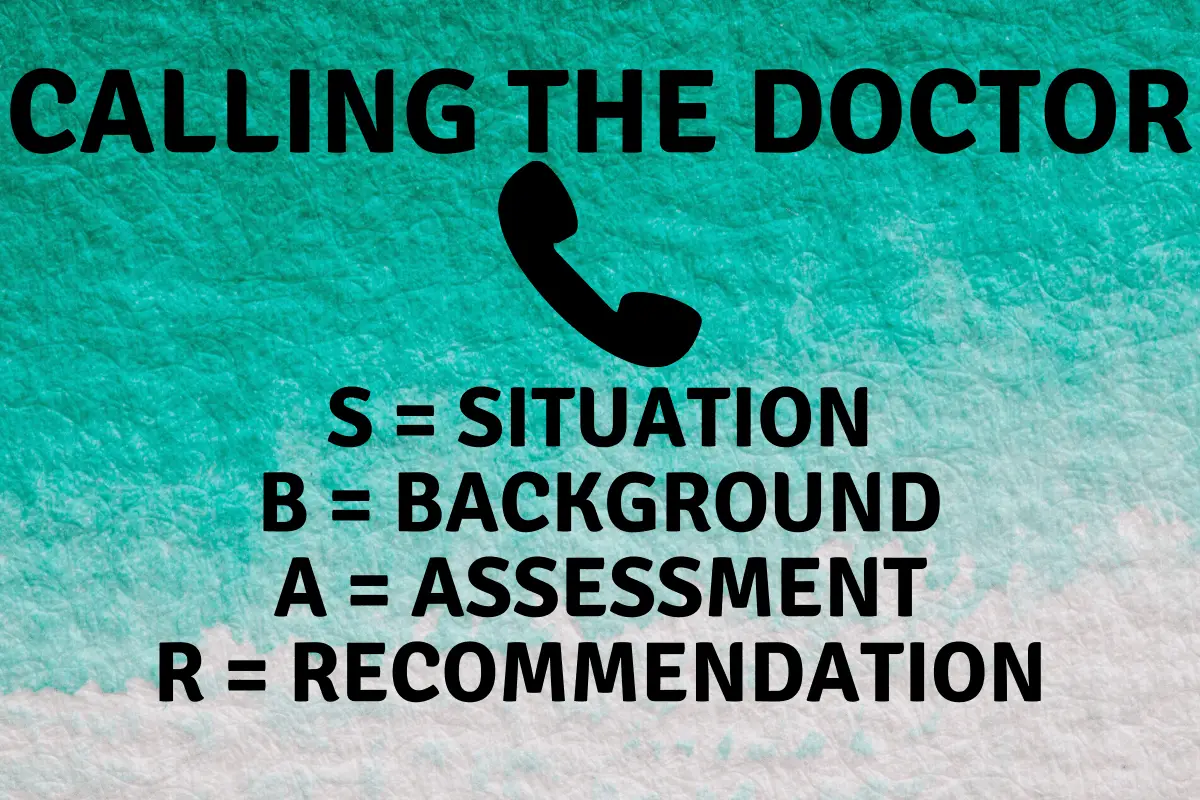
Many facilities use what’s called an SBAR, which stands for situation, background, assessment, and recommendation. This form is supposed to assist the nurse in providing concise and focused information when reporting to another medical professional.
As the structure is shared, it also helps staff anticipate the information needed by colleagues and encourages assessment skills. Using SBAR prompts staff to formulate information with the right level of detail. (ACT Academy for their Quality, Service Improvement and Redesign suite of programmes)
Having some structure that a nurse follows when reporting can help new inexperienced nurses. It also helps calm nurses when they have anxiety about calling “the Doctor.” It gives framework and preparation to have what is needed for the call.
Advantages to using a structured reporting format
Having a structured format for reporting allows for improved communication. Many times when patients are not doing well, it is easy to get overwhelmed.
Anxiety, worry, lack of knowledge can cause a medical professional not properly to inform a medical professional of what is occurring.
You may miss important points in your reporting that could lead to incorrect treatment of the patient. The use of SBAR and other structured reporting has been shown to help reduce medication errors.
Structured reporting can also help improve the relationship between nurses and medical providers. Most medical providers appreciated a well thought out report. It makes the providers less resistant to the call. The nursing report will be more straightforward when it is short, to the point, and helps them come up with a plan of action.
You are calling a doctor at 1 am to report on a patient with chest pain. The following information should be collected before calling.
Is the pain radiating down the patient’s left arm?
Is the pain reproducible?
Does the patient have a cough?
Vitals stable?
When did the pain start?
What is the patient’s health history?
Any cardiac history?
Then with minimal emotion, you explain what you feel the patient is experiencing and make recommendations based on your assessment.
Listen to the doctor’s recommendations and write down the orders. You may have to read back the orders to make sure you didn’t misinterpret the orders.
All this is done in a concise yet thorough way. By getting to the point, you allow the provider to care for the patient in the best way possible. It also allows you to get the best orders to provide care for your patients.
Why not use a structured reporting format?
Many nurses and providers say it would be to difficult to change to an SBAR format for reporting. There are comments such as “It takes too much time” or “The doctor doesn’t want to hear all this information.”
There is also a culture within facilities that can be challenging to change. “We have always done it this way” mentality can lead to resistance from nursing staff and providers.
There is also the time commitment when it comes to training the staff in the use of the SBAR format or something similar. The training requires team members that can show others how to use the form.
The trainers for the new formats will have to review the systems with the nurses and help them become comfortable calling the providers.
Can SBAR be modified?
The short answer is, “Of course it can!”. Try to learn the components of the SBAR format and then modify it to what you feel you could do in the time frame that you have.
Simply having a format to follow trains your mind to have the needed facts to present to the medical provider and obtain the proper orders to keep your patient healthy or prevent further decline.
You will also learn that certain doctors, APRNs, and PAs will have an abbreviated version of what information they like to receive.
Even when providing minimal information, you should still try to follow the format. When making the call:
Situation:
- Who are you?
- Where are you calling from?
- Who are you calling about?
- Why are you concerned?
- Be prepared to answer questions regarding vitals, code status, when did symptoms start? How is the patient feeling now?
Background:
- Why is the patient at the facility?
- Have access to their diagnosis, medications, and laboratories.
- You don’t need to know everything about the patient but have the EHR or chart available to answer the questions.
Assessment:
- The assessment is your moment to shine
- Evaluation of the patient before calling the medical provider
- Come up with a list of symptoms that you have identified during your exam
- Identify any changes from the norm even if you don’t feel it is related (you don’t have to report this unless there is an opportunity)
- Get a fresh set of vital signs.
- Start reporting with what worries you the most then slowly work down from there.
Recommendation:
- Do not be shy in asking for what you think the patient needs.
- Make recommendations for further care if you feel the doctor is missing something.
- Make sure to write down and clarify any orders the provider orders.
- If you don’t know what the doctor is ordering or why, then ask the provider to clarify.
You may find that using the SBAR format is too time-consuming to follow. However, you should always utilize a structured way of reporting.
What is the bare minimum that you will need when calling to give a report?
- Name of patient
- The facility you are calling from
- What are allergies
- Name of patient
- What prompted you to call
- Your assessment
- Any chronic kidney disease or liver disease (to help with picking medications)
- Have access to the chart and EHR
- Pen and paper to take down orders
Basic assessment of the patient before calling a medical provider
Before calling the provider, there should always be an assessment of the patient. This assessment should be completed by the one calling the provider whenever possible.
There will be necessary information that is needed and usually requires laying your eyes on the patient and assessing the patient. Focus your assessment on what you think is causing the patient’s symptoms.
A quick way to assess the patient is to identify the problem and evaluate that system. Then assess the system above and below. For example, if coughing, listen to the chest, then neck (with palpation of the area), and then listen and palpate the abdomen. This assessment is the bare minimum that should be done before calling.
There will be times when there isn’t time to call the doctor or APRN, such as when a nurse calls the supervisor from another floor due to coding residents.
An actively dying resident requires the patient to be sent out immediately, and any delay in calling 911 would cause potential harm to the resident.
However, most times, there is time for the supervisor or nurse to do a proper assessment. The nurse will be the eyes and ears of the doctor. The nurse will need to be able to explain what they see to the doctor so that an accurate decision can, regarding the patient’s care.
How to present yourself when making the call to the medical provider
When you are making the call to the provider, introduce yourself as someone who knows what you’re talking about. Never call in “panic mode,” even if you are worried about your patient.
Call with a tone of confidence so that you can present the facts in a clear and succinct way.
Talk with confidence even if you have self-doubt. One way to do this is to spend the time getting the necessary information before calling. By preparing, you can answer the questions the doctor may have.
Conclusion:
The days of old of the doctors yelling at the nurses during the report are rarer than ten years ago. Most facilities will not tolerate a rude doctor, APRN, or Physician Assistant.
Facilities will expect the provider to return the same level of respect that the nurse shows them. The expectation of respect doesn’t mean that you shouldn’t care how you speak with the doctor, it just means you should be less afraid to make the call when prepared.
You are calling the provider to stop an adverse event from happening to the patient. Call with the knowledge that you are doing the right thing for the patient.